
Lower Back Pain

Mechanical Back Pain
Mechanical back pain refers to discomfort or pain in the lower back resulting from issues related to the spine’s structure and function. This type of pain often arises from muscle strains, ligament sprains, or herniated discs, and is commonly linked to activities such as lifting heavy objects, poor posture, or prolonged sitting. Mechanical back pain typically manifests as a dull, aching sensation or sharp pain that may improve with rest and worsen with movement or certain positions. Treatment often includes physical therapy, ergonomic adjustments, and exercises to strengthen the back and improve flexibility.
Degenerative Disc Diseases
Degenerative disc disease is a condition where the intervertebral discs in the lower back undergo wear and tear over time, leading to pain and discomfort. As the discs age, they can lose hydration, elasticity, and height, which diminishes their ability to cushion the vertebrae and absorb shock. This degeneration can cause back pain, stiffness, and reduced mobility, and may lead to conditions like herniated discs or spinal stenosis. Symptoms often include chronic lower back pain that worsens with activity and improves with rest. Treatment typically focuses on pain management, physical therapy, and lifestyle changes to support spinal health and alleviate symptoms.


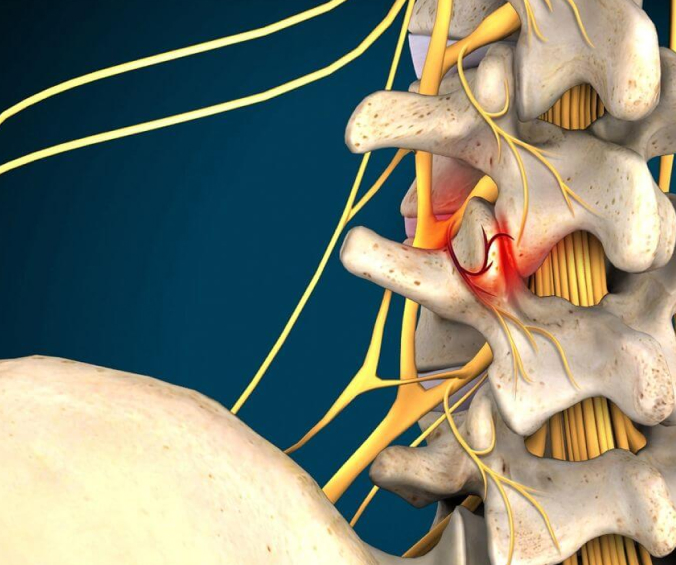
Disc Herniation
Disc herniation occurs when the soft, gel-like center (nucleus pulposus) of an intervertebral disc in the lower back pushes through a tear in the tougher outer layer (annulus fibrosus). This herniation can press on nearby nerves, causing pain, numbness, or weakness in the lower back, buttocks, and legs. Symptoms often include sharp or shooting pain that may worsen with movement, coughing, or sneezing. Herniated discs can result from age-related degeneration, trauma, or repetitive strain. Treatment generally involves conservative measures such as physical therapy, medications, and lifestyle adjustments, though severe cases may require surgical intervention to relieve nerve pressure and restore function.
Facet Joint Arthritis
Facet joint arthritis, also known as facet arthropathy, is a condition where the facet joints in the lower back, which are responsible for stabilizing and guiding spine movement, become inflamed and degenerate over time. This arthritis leads to pain, stiffness, and reduced mobility in the lower back, often exacerbated by activities that involve bending, twisting, or prolonged standing. Symptoms may include a dull, aching pain that radiates to the buttocks or thighs, and increased discomfort with certain movements or postures. Treatment typically focuses on pain relief and improving function through physical therapy, medications, and sometimes injections. In severe cases, surgical options may be considered to alleviate symptoms and improve quality of life.

Spinal Stenosis
Spinal stenosis is a condition characterized by the narrowing of the spinal canal, which compresses the spinal cord and nerves in the lower back. This narrowing can result from age-related changes, such as degenerative disc disease or thickening of the spinal ligaments, or from conditions like arthritis. Symptoms of spinal stenosis may include lower back pain, leg pain, numbness, or weakness, which often worsen with walking or standing and improve with rest or sitting. Treatment typically involves physical therapy, pain management, and lifestyle modifications to alleviate symptoms and improve mobility. In more severe cases, surgical interventions may be considered to relieve nerve compression and restore spinal function.
Compression Fractures
Compression fractures occur when the vertebrae in the lower back collapse due to loss of bone density, trauma, or other conditions that weaken the bones. These fractures can cause sudden, sharp pain in the lower back, which may be aggravated by movement, lifting, or prolonged standing. In addition to pain, compression fractures can lead to a loss of height and a hunched posture. Common causes include osteoporosis, where bones become brittle and weak, or trauma such as a fall or accident. Treatment often focuses on managing pain with medications, physical therapy to strengthen and support the back, and, in some cases, surgical interventions such as vertebroplasty or kyphoplasty to stabilize the fractured vertebra and relieve symptoms.


Sacroiliac Region Pain
Sacroiliac (SI) region pain originates from the sacroiliac joints, which connect the base of the spine (sacrum) to the pelvis (ilium). This type of lower back pain is often characterized by discomfort in the lower back and buttocks, which may also radiate to the thighs or groin. SI joint pain can be caused by factors such as joint dysfunction, inflammation, or injury, and may be exacerbated by activities that involve standing for long periods, lifting, or twisting motions. Common symptoms include sharp or aching pain, stiffness, and limited mobility. Treatment usually involves physical therapy to improve joint stability and strength, pain management with medications or injections, and lifestyle modifications to reduce strain on the SI joint.
